U.S. Healthcare Cybersecurity Threats Surge 25%: Patient Data at Risk

A new report details a concerning 25% surge in U.S. healthcare cybersecurity threats over the past three months, directly impacting the security and privacy of patient data across the nation.
The landscape of healthcare in the United States is constantly evolving, and with technological advancements comes an increased vulnerability to digital threats. A recent report has unveiled a stark reality: U.S. healthcare cybersecurity threats have surged by an alarming 25% in just the last three months, raising critical questions about patient data protection.
understanding the recent surge in cyberattacks
The recent increase in cyberattacks targeting the U.S. healthcare sector is not merely a statistical anomaly; it represents a growing, sophisticated threat to sensitive patient information. This surge encompasses a variety of attack vectors, from ransomware demanding hefty payments to data breaches exposing millions of patient records.
Understanding the root causes behind this escalation is crucial for developing effective countermeasures. Several factors contribute to the healthcare industry’s heightened vulnerability, including an expanded digital footprint and often outdated security infrastructures.
key factors driving the increase
Several elements are converging to create a perfect storm for cybercriminals targeting healthcare organizations. These factors range from the sheer volume of valuable data to the operational criticalities of healthcare systems.
- High-Value Data: Patient health information (PHI) is a goldmine for attackers, often containing personally identifiable information (PII), financial details, and medical histories, all highly valuable on the dark web.
- Legacy Systems: Many healthcare providers still rely on older, less secure IT systems that are difficult to patch and protect against modern threats.
- Interconnected Ecosystems: The vast network of third-party vendors, medical devices, and cloud services creates numerous entry points for attackers.
- Ransomware as a Service (RaaS): The proliferation of RaaS models makes it easier for less technically skilled individuals to launch sophisticated attacks.
The complexity of healthcare IT environments, coupled with a critical need for uninterrupted service, makes these institutions particularly attractive targets. Downtime due to a cyberattack can have immediate and severe consequences for patient care, often pressuring organizations to pay ransoms.
In conclusion, the surge in cyberattacks is a multifaceted problem driven by the lucrative nature of healthcare data, technological limitations, and the evolving tactics of cybercriminals. Addressing this requires a comprehensive strategy that tackles these underlying issues head-on.
the direct impact on patient data and privacy
When cyberattacks penetrate healthcare defenses, the immediate and most severe consequence is the compromise of patient data. This isn’t just about abstract numbers; it’s about real people whose most private information can be exposed, leading to significant personal and financial repercussions.
The integrity and confidentiality of patient records are foundational to trust in the healthcare system. Breaches erode this trust, making individuals hesitant to share vital information, which can ultimately affect the quality of care they receive.
types of data exposed and their consequences
Patient data is incredibly diverse, and different types of exposed information carry varying risks. Attackers often seek a comprehensive profile for identity theft or fraudulent medical claims.
When patient data is compromised, the fallout can be extensive. Individuals might face:
- Identity Theft: Criminals use stolen personal details to open fraudulent accounts, obtain loans, or commit other financial crimes.
- Medical Identity Theft: This occurs when someone uses another person’s identity to obtain medical services, potentially leading to incorrect medical records and billing issues.
- Blackmail and Extortion: Highly sensitive medical conditions can be used to extort individuals, causing immense psychological distress.
- Financial Hardship: Victims may incur out-of-pocket expenses to resolve issues stemming from data breaches, such as credit monitoring or legal fees.
Furthermore, the long-term psychological impact on individuals whose medical privacy has been violated can be profound. The feeling of vulnerability and loss of control over personal health information is a significant, often overlooked, consequence.
The direct impact on patient data extends beyond immediate financial or identity-related concerns. It fundamentally undermines the patient-provider relationship and the broader public’s confidence in the ability of healthcare institutions to safeguard their most sensitive information. Protecting this data is not just a regulatory requirement; it is an ethical imperative.
vulnerable points in healthcare cybersecurity infrastructure
The healthcare sector’s cybersecurity infrastructure is vast and complex, encompassing everything from electronic health records (EHR) systems to networked medical devices. This intricate web presents numerous vulnerable points that cybercriminals are adept at exploiting.
Identifying these weaknesses is the first step toward building a more resilient defense. Many vulnerabilities stem from the rapid adoption of new technologies without commensurate security upgrades, as well as human factors.
common entry points for attackers
Attackers often target the weakest links in a system. In healthcare, these can be surprisingly diverse, requiring a multi-layered security approach.
- Phishing and Social Engineering: Employees remain a primary target for phishing attacks, which trick them into revealing credentials or installing malware.
- Unpatched Software and Systems: Outdated operating systems and applications with known vulnerabilities are easily exploited by automated tools.
- Weak Authentication: Lack of multi-factor authentication (MFA) leaves accounts susceptible to brute-force attacks or stolen credentials.
- Medical Devices and IoT: Many internet-connected medical devices (IoMT) are designed with functionality over security, creating backdoors into hospital networks.
- Third-Party Vendors: Supply chain attacks through less secure third-party service providers are increasingly common, as seen in numerous recent breaches.
The sheer number of endpoints, from workstations to mobile devices used by staff, further complicates security efforts. Each device represents a potential vector for attack, requiring constant vigilance and robust management.
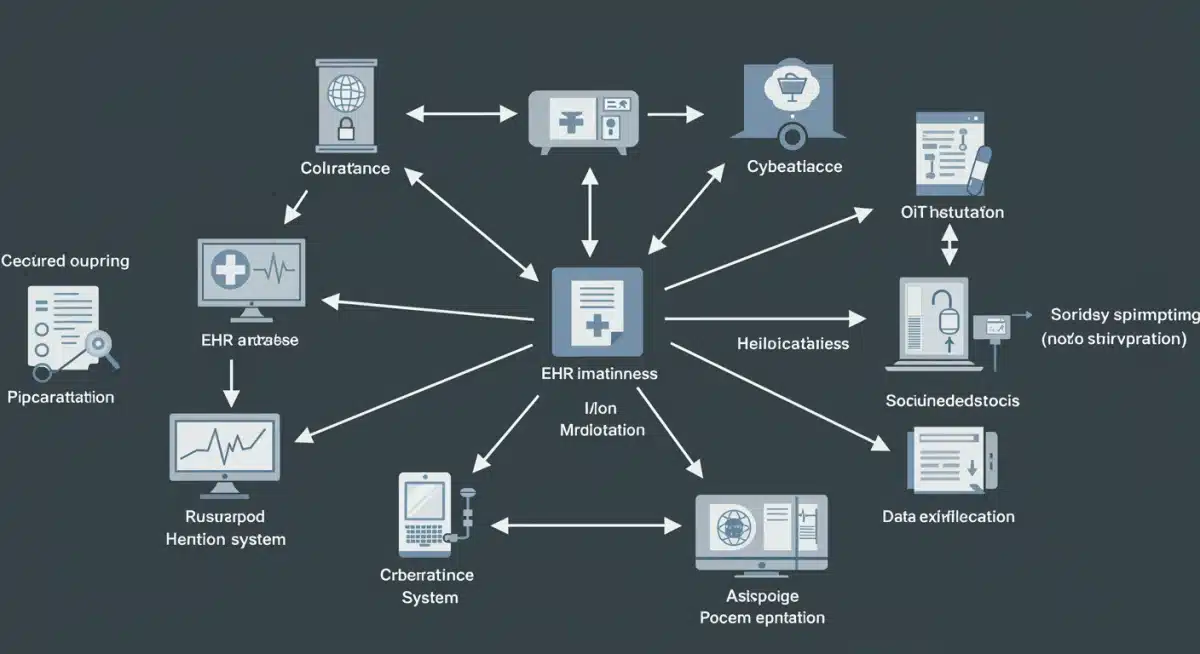

The conclusion is clear: a holistic approach to security is needed, one that addresses not only technological gaps but also human behavior and the interconnectedness of the entire healthcare ecosystem. Ignoring any single vulnerable point leaves the entire system at risk.
regulatory responses and ongoing challenges
In response to escalating U.S. healthcare cybersecurity threats, regulatory bodies have pushed for stronger compliance and accountability. The Health Insurance Portability and Accountability Act (HIPAA) remains the cornerstone, but its enforcement and adaptation to new threats are constant challenges.
HIPAA’s Security Rule mandates administrative, physical, and technical safeguards to protect electronic protected health information (ePHI). However, merely complying with minimum requirements is often insufficient against sophisticated cyber adversaries.
evolving HIPAA and other compliance frameworks
The regulatory landscape is continually evolving, with new guidelines and interpretations aimed at bolstering cybersecurity. Organizations must stay abreast of these changes to avoid penalties and genuinely protect patient data.
- HIPAA Enforcement: The Office for Civil Rights (OCR) actively investigates breaches and imposes significant fines for non-compliance, pushing organizations to prioritize security.
- State-Specific Regulations: Beyond federal mandates, states are enacting their own data privacy laws, adding layers of complexity for multi-state healthcare providers.
- NIST Cybersecurity Framework: Many organizations adopt frameworks like NIST (National Institute of Standards and Technology) to establish more robust and proactive security programs.
- Information Sharing: Encouraging the sharing of threat intelligence among healthcare organizations helps to anticipate and mitigate emerging threats more effectively.
Despite these efforts, significant challenges persist. The sheer volume of data, the rapid pace of technological change, and the constant evolution of cyber threats make achieving and maintaining full compliance a daunting task. Furthermore, smaller healthcare providers often lack the resources to implement comprehensive security measures.
Ultimately, while regulatory frameworks provide a necessary baseline, achieving true cybersecurity resilience requires a commitment to continuous improvement, investment in advanced technologies, and a culture of security awareness that extends throughout the entire organization.
strategies for enhancing healthcare cybersecurity
Given the escalating nature of U.S. healthcare cybersecurity threats, organizations must adopt proactive and comprehensive strategies to safeguard patient data. A reactive approach is no longer sustainable; instead, a multi-layered defense-in-depth strategy is essential.
Effective cybersecurity in healthcare involves a combination of technological solutions, robust policies, and continuous staff training. It’s about creating a resilient ecosystem that can detect, prevent, and respond to attacks efficiently.
implementing robust security measures
Hospitals and clinics need to invest in a range of security measures that cover all potential attack vectors. This includes both foundational security practices and advanced threat detection capabilities.
- Multi-Factor Authentication (MFA): Implementing MFA across all systems significantly reduces the risk of unauthorized access due to stolen credentials.
- Regular Vulnerability Assessments and Penetration Testing: Proactively identify and remediate weaknesses before attackers can exploit them.
- Employee Training and Awareness: Educate staff on phishing, social engineering, and safe data handling practices to turn them into the first line of defense.
- Incident Response Plans: Develop and regularly test comprehensive plans to minimize damage and recovery time in the event of a breach.
- Data Encryption: Encrypting data both in transit and at rest adds a critical layer of protection, making compromised data unreadable without the correct keys.
- Network Segmentation: Dividing networks into smaller, isolated segments can limit the spread of an attack if one part of the system is compromised.
The importance of robust backup and recovery systems cannot be overstated, especially in the face of ransomware attacks. The ability to restore operations quickly and reliably is paramount for patient care continuity.
In conclusion, enhancing healthcare cybersecurity is an ongoing journey that requires sustained investment, strategic planning, and a commitment to adapting to new threats. By implementing these robust measures, healthcare organizations can significantly improve their resilience against cyberattacks and better protect patient data.
the role of insider knowledge and threat intelligence
In the battle against cyberattacks, insider knowledge and robust threat intelligence play an increasingly vital role. Understanding the tactics, techniques, and procedures (TTPs) of adversaries, alongside insights from past incidents, can significantly bolster an organization’s defensive posture.
This isn’t just about external reports; it’s also about leveraging internal data, incident logs, and employee observations to identify patterns and potential vulnerabilities before they are exploited.
leveraging data for proactive defense
Proactive defense relies heavily on the ability to gather, analyze, and act upon relevant information. This includes both broad industry trends and specific organizational insights.
- Threat Intelligence Platforms: Subscribing to and actively using platforms that provide real-time information on emerging threats, vulnerabilities, and attack campaigns.
- Internal Security Audits: Conducting regular, thorough internal audits to identify misconfigurations, unauthorized access, and policy violations.
- Security Information and Event Management (SIEM): Implementing SIEM systems to aggregate and analyze security logs from various sources, helping to detect suspicious activities.
- Endpoint Detection and Response (EDR): Deploying EDR solutions to monitor endpoints for malicious activity and provide capabilities for rapid response.
- Collaboration and Information Sharing: Participating in industry-specific information-sharing and analysis organizations (ISAOs) to benefit from collective knowledge and early warnings.
The human element of insider knowledge extends beyond just malicious actors; it also includes the valuable insights that IT security professionals and even general staff can provide regarding system behavior and potential anomalies. Encouraging a culture where employees feel comfortable reporting suspicious activities without fear of reprisal is critical.
In essence, harnessing insider knowledge and external threat intelligence transforms a reactive security stance into a proactive one. This allows healthcare organizations to anticipate attacks, strengthen their defenses strategically, and ultimately protect patient data more effectively against the ever-evolving landscape of cyber threats.
| Key Point | Brief Description |
|---|---|
| Threat Surge | U.S. healthcare cybersecurity threats increased by 25% in the last three months, raising urgent concerns. |
| Patient Data Impact | Compromised patient data leads to identity theft, medical fraud, and significant personal distress. |
| Vulnerability Areas | Legacy systems, third-party vendors, and medical IoT devices are common weak points for attackers. |
| Defense Strategies | MFA, employee training, incident response plans, and data encryption are crucial for protection. |
frequently asked questions about healthcare cybersecurity
The surge is driven by the high value of patient data, the prevalence of legacy IT systems, interconnected healthcare ecosystems, and the accessibility of ransomware-as-a-service models for cybercriminals seeking financial gain and disruption.
Direct impacts include identity theft, medical identity theft leading to fraudulent services, potential blackmail from sensitive health information exposure, and significant financial hardships due to recovery efforts and associated costs.
While HIPAA provides a foundational framework, compliance alone is often insufficient against sophisticated modern threats. Continuous adaptation, proactive measures, and adherence to advanced frameworks like NIST are increasingly necessary to ensure robust protection.
Effective strategies include implementing multi-factor authentication, conducting regular vulnerability assessments, comprehensive employee training, developing robust incident response plans, and encrypting sensitive data both in transit and at rest.
Insider knowledge, combined with external threat intelligence, allows organizations to proactively identify vulnerabilities and anticipate attacks. It leverages internal audits, SIEM systems, EDR solutions, and fosters a culture where employees report suspicious activities, enhancing overall defense.
conclusion
The alarming 25% surge in U.S. healthcare cybersecurity threats over the past three months underscores an urgent need for reinforced digital defenses. The implications for patient data are profound, ranging from identity theft to eroded trust in healthcare providers. As cybercriminals grow more sophisticated, healthcare organizations must move beyond basic compliance, adopting comprehensive strategies that include advanced technological safeguards, continuous staff education, and the strategic utilization of threat intelligence. Protecting patient privacy is not merely a technical challenge but a critical ethical responsibility that demands ongoing vigilance and investment from every entity within the healthcare ecosystem. Only through a unified and proactive approach can the industry hope to shield its most valuable asset: patient information.





