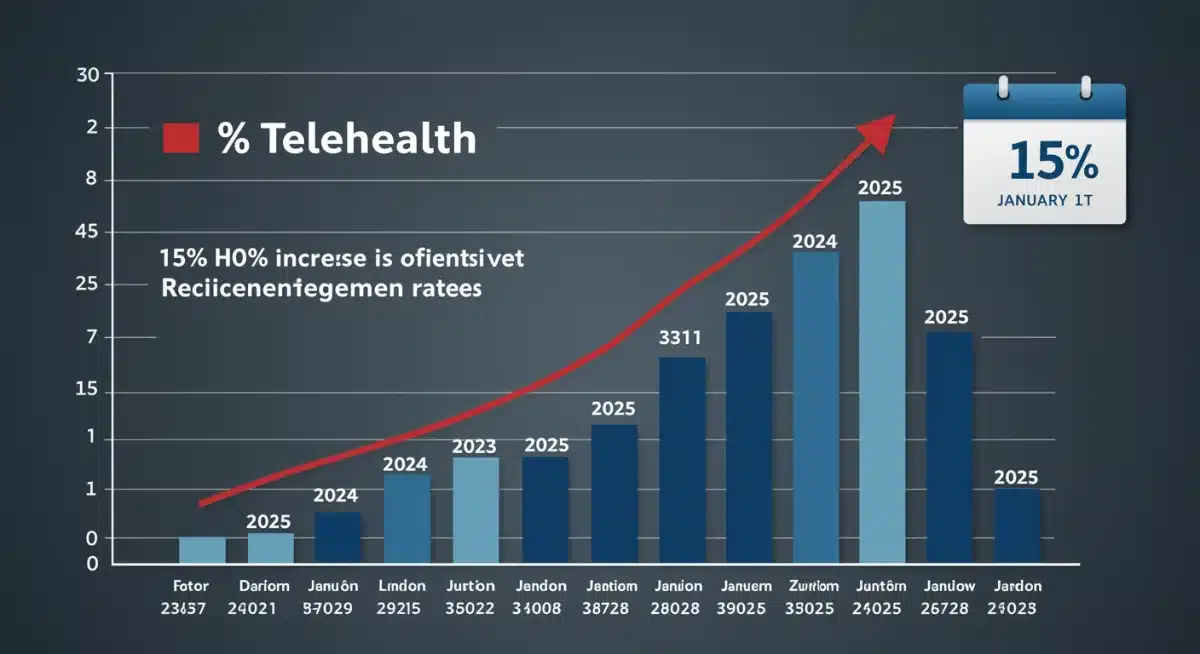
CMS Announces 15% Telehealth Reimbursement Increase for 2025

The Centers for Medicare & Medicaid Services (CMS) has announced a crucial 15% increase in telehealth reimbursement rates, effective January 1, 2025, signaling a substantial shift in healthcare delivery and access.
The healthcare landscape is continuously evolving, and a recent announcement from the Centers for Medicare & Medicaid Services (CMS) marks a pivotal moment for virtual care. Effective January 1, 2025, CMS will implement a 15% increase in telehealth reimbursement rates for 2025, a decision poised to significantly impact providers, patients, and the future of healthcare delivery across the United States. This time-sensitive update underscores a growing commitment to integrating telehealth into the mainstream of medical practice.
Understanding the CMS Decision on Telehealth Reimbursement
The Centers for Medicare & Medicaid Services (CMS) has made a landmark decision by announcing a 15% increase in telehealth reimbursement rates for 2025. This move is not merely an adjustment in payment; it represents a strategic endorsement of telehealth’s role in modern healthcare. The increase aims to stabilize and expand access to virtual care services, recognizing their critical importance in patient management and chronic disease care, especially in underserved areas.
This decision comes after extensive evaluation of telehealth’s performance, patient outcomes, and provider experiences during the recent public health emergency. CMS has been gathering data and feedback to inform policies that best serve the American public while ensuring the sustainability of healthcare systems. The 15% increase is a direct response to these findings, designed to encourage broader adoption and appropriate utilization of telehealth services.
The Rationale Behind the Rate Hike
Several factors contributed to CMS’s decision to boost telehealth reimbursement. Foremost among these is the undeniable evidence of telehealth’s effectiveness in maintaining continuity of care, reducing hospital readmissions, and improving patient satisfaction. The pandemic accelerated telehealth adoption, revealing its potential to overcome geographical barriers and enhance access to specialists.
- Enhanced Access: Telehealth significantly broadens access to healthcare, particularly for individuals in rural or remote areas who face challenges reaching physical clinics.
- Improved Patient Outcomes: Studies have shown that virtual care can lead to better management of chronic conditions and timely interventions.
- Operational Efficiency: For providers, telehealth can streamline operations, reduce overheads, and optimize scheduling, allowing more patients to be seen.
Furthermore, the increase reflects an understanding of the technological and infrastructural investments providers have made to implement and maintain telehealth capabilities. By increasing reimbursement, CMS aims to validate these investments and incentivize further innovation in virtual care delivery. This will ensure that the quality of care provided remotely meets or exceeds the standards of in-person visits.
Impact on Healthcare Providers and Systems
For healthcare providers, the 15% increase in telehealth reimbursement rates for 2025 is a significant financial boost that could reshape their operational models. This adjustment provides greater financial stability for practices that have invested heavily in virtual care infrastructure and training. It also offers an incentive for those who have been hesitant to fully embrace telehealth due to previous reimbursement uncertainties.
The increased rates mean that providers can expect more equitable compensation for virtual services, bringing them closer to parity with in-person visits. This can alleviate some of the financial pressures associated with maintaining a robust telehealth program, from technology costs to staffing for virtual care coordination. It also encourages providers to expand their telehealth offerings, reaching more patients and potentially reducing appointment backlogs.
Operational Changes and Strategic Planning
With the new rates, providers will need to re-evaluate their current telehealth strategies. This includes assessing their technology platforms, staff training needs, and patient engagement approaches. The goal will be to maximize the benefits of increased reimbursement while continuing to deliver high-quality, patient-centered care. Strategic planning will involve integrating telehealth more deeply into the overall care continuum.
- Technology Upgrades: Investing in more advanced telehealth platforms and secure communication tools.
- Staff Training: Ensuring clinical and administrative staff are proficient in virtual care delivery and billing.
- Workflow Optimization: Streamlining processes for virtual appointments, from scheduling to follow-up.
This financial incentive is expected to drive further innovation in telehealth. Providers might explore new virtual services, implement remote monitoring solutions, or develop specialized telehealth programs for specific patient populations. The increased reimbursement fosters an environment where healthcare organizations can confidently invest in the future of digital health, ultimately leading to more accessible and efficient care delivery.
Benefits for Patients: Enhanced Access and Convenience
The CMS telehealth reimbursement 2025 increase is not just a win for providers; it’s a monumental step forward for patients across the United States. Enhanced reimbursement rates directly translate into expanded access to care, greater convenience, and potentially lower out-of-pocket costs for many individuals. This move solidifies telehealth as a viable and valuable option for receiving medical attention.
Patients will likely see a broader range of specialists and primary care providers offering telehealth services. This is particularly beneficial for those in rural areas, individuals with mobility issues, or those who struggle to take time off work for appointments. The convenience of consulting a doctor from home eliminates travel time, parking costs, and the need for childcare, making healthcare more manageable and less disruptive to daily life.
Addressing Disparities and Improving Health Equity
One of the most profound impacts of increased telehealth reimbursement is its potential to address health disparities. By making virtual care more financially sustainable for providers, CMS is helping to ensure that quality healthcare is available to a wider demographic, regardless of socioeconomic status or geographic location. This can lead to improved health equity and better outcomes for underserved communities.
- Reduced Travel Burden: Patients in remote areas can access specialists without long, arduous journeys.
- Greater Flexibility: Appointments can be scheduled more easily around work and family commitments.
- Continuity of Care: Easier follow-ups and chronic disease management through virtual visits.
Moreover, the increased adoption of telehealth encouraged by these rates can lead to earlier detection and management of health conditions. Patients who might have delayed seeking care due to logistical challenges or cost concerns may now find it easier to connect with a provider. This proactive approach to health can prevent conditions from worsening and improve overall public health outcomes. The focus remains on patient-centered care, ensuring that virtual visits are as effective and engaging as in-person consultations.
Navigating the New Reimbursement Landscape: What Providers Need to Know
The upcoming 15% increase in CMS telehealth reimbursement 2025 rates necessitates a thorough understanding of the new landscape for healthcare providers. It is crucial for practices to stay abreast of the specific codes, billing guidelines, and documentation requirements that will accompany these changes. Missteps in billing can lead to revenue loss and compliance issues, undermining the benefits of the rate hike.
Providers should proactively review the official CMS guidelines and any accompanying sub-regulatory guidance as they are released. This includes understanding which services are eligible for the increased reimbursement, the specific modalities that are covered (e.g., audio-only, audio-video), and any patient consent requirements. Staying informed will ensure that practices can accurately bill for services and maximize their financial returns.
Key Considerations for Implementation
Beyond just understanding the new rates, successful implementation requires a holistic approach to telehealth integration. This means evaluating current technological capabilities, ensuring staff are adequately trained in new billing procedures, and communicating clearly with patients about available telehealth options. The goal is to seamlessly incorporate these changes into existing workflows.
- Billing and Coding Updates: Train billing staff on the new CPT and HCPCS codes and modifiers specific to telehealth.
- Documentation Standards: Ensure clinical documentation accurately reflects the virtual nature of the visit and medical necessity.
- Compliance: Stay updated on all federal and state regulations regarding telehealth, including licensing and privacy laws.
Providers should also consider investing in robust electronic health record (EHR) systems that can effectively manage telehealth appointments and integrate billing processes. This technological backbone will be essential for efficient operations and accurate record-keeping in the new reimbursement environment. By preparing thoroughly, providers can fully leverage the increased rates to enhance their service offerings and financial health.
Future Outlook: Telehealth’s Evolving Role in Healthcare
The 15% increase in telehealth reimbursement rates for 2025 is more than just a temporary measure; it signals a long-term commitment from CMS to integrate virtual care permanently into the healthcare ecosystem. This decision paves the way for further innovation and expansion of telehealth services, transforming how patients access and receive medical care in the years to come.
We can expect to see continued growth in specialized telehealth programs, such as remote mental health services, virtual physical therapy, and telemonitoring for chronic conditions. The financial stability offered by increased reimbursement will encourage healthcare organizations to develop more sophisticated and comprehensive virtual care models, moving beyond simple video consultations to integrated digital health solutions.
Anticipated Trends and Innovations
The future of telehealth will likely involve greater integration of artificial intelligence (AI) and machine learning to personalize care, predict health outcomes, and optimize provider workflows. Wearable technology and remote patient monitoring devices will become even more prevalent, providing continuous health data that can be analyzed virtually to inform treatment plans.
- AI-Powered Diagnostics: AI tools assisting in virtual diagnoses and treatment recommendations.
- Hybrid Care Models: A blend of in-person and virtual visits becoming the standard of care.
- Expanded Service Offerings: New types of medical and wellness services delivered remotely.
Furthermore, policy discussions will likely continue around interstate licensing for telehealth providers, data interoperability, and equitable access to broadband internet, all crucial for maximizing telehealth’s potential. The CMS decision is a critical step, but it is part of a larger, ongoing effort to modernize healthcare. The ultimate goal is a more resilient, accessible, and patient-centered healthcare system that leverages technology to its fullest.
Preparing for January 1, 2025: A Time-Sensitive Call to Action
With the effective date of January 1, 2025, rapidly approaching, the announcement of a 15% increase in CMS telehealth reimbursement 2025 rates serves as a time-sensitive call to action for all stakeholders in the healthcare industry. Proactive preparation is essential to seamlessly transition to the new reimbursement structure and fully capitalize on its benefits. Waiting until the last minute could result in missed opportunities and operational challenges.
Healthcare organizations, individual providers, and even technology vendors should begin their preparations now. This involves conducting internal audits of current telehealth practices, identifying areas for improvement, and allocating resources for necessary upgrades and training. The sooner these preparations begin, the smoother the transition will be, ensuring that patient care remains uninterrupted and revenue streams are optimized.
Strategic Steps for Readiness
The transition requires a multi-faceted approach, encompassing financial, operational, and technological readiness. Engaging key personnel from different departments—clinical, administrative, IT, and billing—will ensure a comprehensive preparation strategy. This collaborative effort will be vital for a successful rollout of the new reimbursement rates.
- Internal Audits: Review current telehealth service utilization, billing practices, and technological infrastructure.
- Stakeholder Communication: Inform staff and patients about the upcoming changes and what they mean for service delivery.
- Resource Allocation: Budget for necessary technology upgrades, staff training, and compliance resources.
- Policy Review: Stay informed about any further CMS guidance or state-level policy changes that may impact telehealth.
By taking these proactive steps, healthcare providers can ensure they are well-positioned to leverage the increased reimbursement rates, expand their telehealth offerings, and continue providing high-quality, accessible care to their communities. The January 1, 2025, deadline is not just a date on the calendar; it’s a milestone marking the next significant phase in the evolution of telehealth in the United States.
| Key Point | Brief Description |
|---|---|
| Reimbursement Increase | CMS announced a 15% increase in telehealth reimbursement rates. |
| Effective Date | New rates become effective on January 1, 2025. |
| Impact on Providers | Provides financial stability and incentivizes expanded virtual care offerings. |
| Patient Benefits | Enhances access, convenience, and health equity for patients. |
Frequently Asked Questions About Telehealth Reimbursement
CMS has announced a 15% increase in reimbursement rates for telehealth services. This significant adjustment aims to support the continued growth and integration of virtual care into the broader healthcare system, ensuring providers are adequately compensated for their remote services and encouraging wider adoption.
The new reimbursement rates for telehealth services, including the 15% increase, are scheduled to take effect on January 1, 2025. Healthcare providers and organizations should prepare for these changes well in advance to ensure a smooth transition and compliance with new billing procedures.
Healthcare providers will experience greater financial stability and incentive to expand their telehealth offerings. The increased rates can help offset technology costs, staffing, and training, making virtual care a more sustainable and attractive option for delivering services and reaching a wider patient base.
Patients will benefit from enhanced access to care, greater convenience, and potentially reduced travel burden and costs. The increase encourages more providers to offer telehealth, improving access to specialists and primary care, especially for those in rural or underserved areas, fostering better health outcomes and equity.
Providers should conduct internal audits of current telehealth practices, update billing and coding procedures, invest in necessary technology upgrades, and ensure staff training. Staying informed about official CMS guidelines and preparing proactively will be crucial for maximizing benefits and ensuring compliance with the new reimbursement structure.
Conclusion
The announcement by CMS of a 15% increase in telehealth reimbursement rates for 2025, effective January 1, marks a pivotal moment for the future of healthcare. This decisive action underscores the growing recognition of telehealth’s indispensable role in delivering accessible, efficient, and high-quality care across the nation. For providers, it offers renewed financial viability and an incentive to innovate, while for patients, it promises expanded access and convenience. As the effective date approaches, proactive preparation and a clear understanding of the evolving landscape will be paramount for all stakeholders to fully harness the transformative potential of this significant policy shift, ultimately fostering a more resilient and patient-centered healthcare system.





