Achieving 100% Competency: MedTech Device Training 2025

Achieving 100% competency in MedTech device training by 2025 is critical for ensuring patient safety, optimizing clinical outcomes, and maintaining compliance with evolving regulatory standards across all healthcare settings.
In the rapidly evolving landscape of healthcare, ensuring that all professionals are proficient in using medical technology is not just an aspiration but a critical necessity. MedTech device training for 2025 demands a proactive, comprehensive strategy to achieve 100% competency, safeguarding patient well-being and optimizing operational efficiency.
Understanding the imperative for 100% competency
The medical technology sector is characterized by continuous innovation, with new devices constantly emerging to enhance diagnostic capabilities, treatment efficacy, and patient care. This rapid advancement, while beneficial, introduces a significant challenge: ensuring that every healthcare professional who interacts with these devices possesses the requisite knowledge and skills to operate them safely and effectively. The imperative for 100% competency stems directly from the need to minimize errors, improve patient safety, and adhere to stringent regulatory guidelines.
Failure to achieve universal competency can have severe repercussions, including adverse patient events, increased operational costs due to device misuse or damage, and potential legal liabilities for healthcare institutions. Furthermore, a lack of confidence in using new technologies can lead to resistance from staff, hindering the adoption of advancements that could otherwise revolutionize care delivery. Therefore, a robust training framework is not merely a compliance exercise but a foundational element of high-quality healthcare.
The evolving regulatory landscape
Regulatory bodies, such as the FDA in the United States, are increasingly emphasizing the importance of user competency in the safe and effective deployment of medical devices. These regulations often require documented proof of training and ongoing assessment to ensure that healthcare providers maintain proficiency over time. Institutions must navigate a complex web of standards, making a systematic approach to training indispensable.
- FDA guidelines: Adherence to current Good Manufacturing Practices (cGMP) and user training requirements.
- Joint Commission standards: Mandates for staff competency in the use of equipment.
- State-specific regulations: Additional requirements that vary by location, necessitating localized training adaptation.
- Risk management: Proactive identification and mitigation of risks associated with device use.
Achieving 100% competency is not a one-time event but an ongoing commitment to excellence. It involves continuous education, regular skill validation, and a culture that prioritizes learning and adaptation. This proactive stance ensures that healthcare organizations remain at the forefront of patient care, capable of leveraging the full potential of modern medical technology.
Strategic planning for MedTech training by 2025
Effective MedTech device training doesn’t happen by chance; it requires meticulous strategic planning. By 2025, healthcare organizations must have well-defined strategies that encompass needs assessment, curriculum development, resource allocation, and a clear roadmap for implementation. This proactive approach ensures that training initiatives are not only comprehensive but also sustainable and scalable to meet future demands.
The planning phase should begin with a thorough analysis of current device usage, identifying gaps in knowledge or skills among staff, and anticipating future technological adoptions. Engaging key stakeholders, including clinical leaders, IT departments, and device manufacturers, is crucial to gather diverse perspectives and ensure the training program aligns with organizational goals and clinical realities.
Conducting a comprehensive needs assessment
A detailed needs assessment is the cornerstone of any successful training program. This involves more than just identifying which devices require training; it delves into understanding who needs training, what specific skills are lacking, and the most effective methods for knowledge transfer. Data can be gathered through surveys, interviews, direct observation, and analysis of incident reports related to device misuse.
- Identify target audience: Delineate roles and departments requiring specific device training.
- Assess current skill levels: Use pre-assessments or existing competency records to pinpoint gaps.
- Prioritize training needs: Focus on high-risk devices or those with significant impact on patient care.
- Analyze learning styles: Tailor training modalities to accommodate diverse learning preferences.
Once the needs are clearly defined, the next step involves designing a curriculum that is both relevant and engaging. This curriculum should not only cover the technical aspects of device operation but also emphasize the clinical context, troubleshooting, and maintenance protocols. By integrating these elements, training becomes more holistic and practical, preparing professionals for real-world scenarios.
Developing an adaptive training curriculum
A static training curriculum quickly becomes obsolete in the fast-paced MedTech environment. For 2025, the focus must be on developing an adaptive curriculum that can evolve with technological advancements and changing clinical practices. This involves incorporating modular designs, leveraging diverse learning methodologies, and ensuring content remains current and relevant to the needs of healthcare professionals.
The curriculum should move beyond traditional classroom lectures, embracing interactive and experiential learning. Simulation-based training, for instance, offers a safe environment for professionals to practice skills and make mistakes without patient risk. Microlearning modules, accessible on-demand, can also provide just-in-time refreshers for specific device functions, supporting continuous learning.
Integrating technology into training delivery
Modern training programs must harness the power of technology to deliver engaging and effective instruction. Learning Management Systems (LMS) can track progress, manage certifications, and provide access to a wealth of educational resources. Virtual reality (VR) and augmented reality (AR) are emerging as powerful tools for immersive training experiences, offering realistic simulations of complex procedures.
- Online modules: Self-paced learning for foundational knowledge and theoretical concepts.
- Simulation labs: Hands-on practice in a controlled environment with realistic scenarios.
- VR/AR training: Immersive experiences for complex device operation and troubleshooting.
- Mobile learning apps: On-demand access to quick guides, tutorials, and refreshers.
Furthermore, the curriculum should emphasize critical thinking and problem-solving skills rather than rote memorization. Healthcare professionals need to understand the ‘why’ behind each step of device operation, enabling them to adapt to unforeseen circumstances and troubleshoot issues effectively. This deeper understanding fosters true competency and confidence in using MedTech devices.
Implementing effective competency assessment and validation
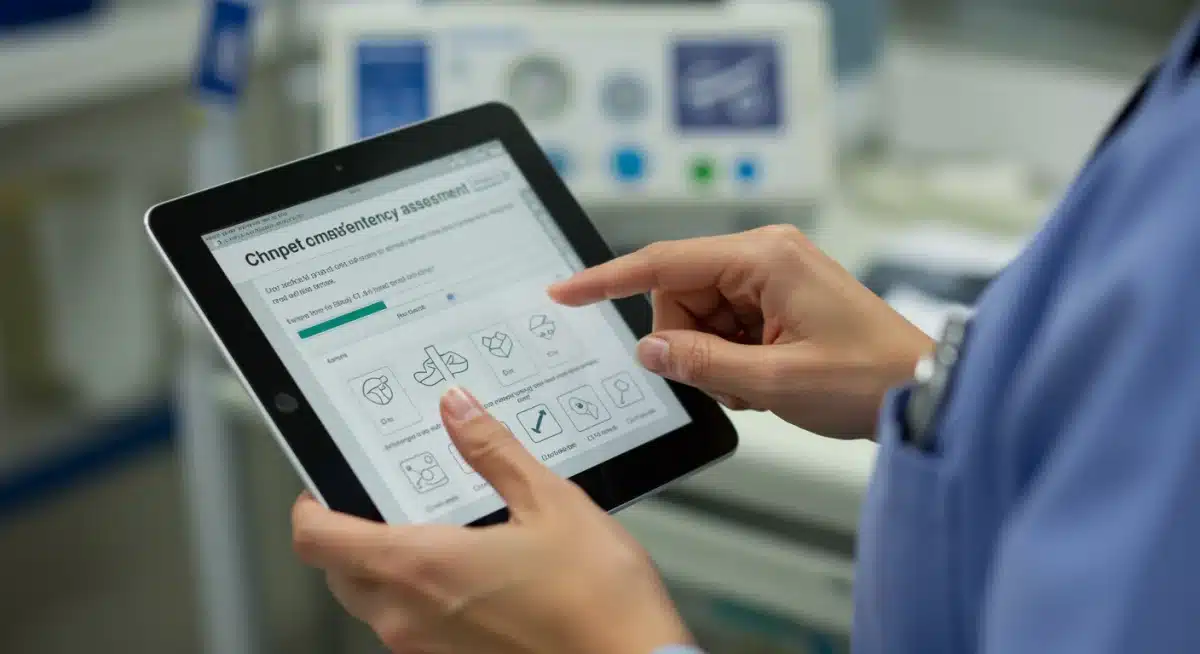
Achieving 100% competency means not only providing training but also rigorously assessing and validating that the knowledge and skills have been acquired and retained. By 2025, assessment methods must be robust, reliable, and integrated into the overall training framework, moving beyond simple checklists to evaluate true proficiency and critical thinking in device usage.
Competency assessment should be multi-faceted, combining theoretical knowledge tests with practical, hands-on evaluations. Direct observation of skills in a clinical or simulated setting is invaluable, allowing trainers to assess not just technical ability but also decision-making, patient interaction, and adherence to safety protocols. Feedback loops are essential, providing constructive criticism and opportunities for improvement.
Utilizing diverse assessment tools
A variety of tools can be employed to effectively assess competency, each offering unique insights into a professional’s understanding and skill level. The choice of assessment tool should align with the specific learning objectives and the complexity of the device being trained on. Regular reassessment is also vital to ensure ongoing proficiency, especially for devices used infrequently or those undergoing software updates.
- Written examinations: To evaluate theoretical knowledge and understanding of device principles.
- Skills checklists: For systematic evaluation of procedural steps during hands-on practice.
- Simulation-based scenarios: To assess critical thinking, problem-solving, and decision-making under pressure.
- Peer-to-peer assessment: Encourages collaborative learning and provides diverse feedback.
Documentation of competency is equally important, not only for regulatory compliance but also for tracking individual progress and identifying areas for further development. Digital platforms can streamline this process, maintaining a comprehensive record of training completion, assessment scores, and certification expiry dates. This ensures accountability and helps in planning future training interventions.
Fostering a culture of continuous learning and improvement
Achieving and maintaining 100% competency in MedTech device training is not a destination but an ongoing journey. By 2025, healthcare organizations must cultivate a culture that champions continuous learning, encourages self-improvement, and views training as an integral part of professional development. This involves creating supportive environments where learning is valued and opportunities for skill enhancement are readily available.
Leadership plays a pivotal role in shaping this culture. When leaders actively participate in training, advocate for continuous education, and recognize achievements, it sends a powerful message to the entire organization. Encouraging open communication about challenges with new devices and providing channels for feedback on training programs can also foster a more responsive and adaptive learning environment.
Implementing ongoing support and refreshers
Initial training, no matter how comprehensive, is rarely sufficient for long-term retention of complex skills. Regular refreshers, access to expert support, and opportunities for advanced training are crucial for sustaining high levels of competency. These ongoing support mechanisms help reinforce learning, address emerging questions, and keep professionals updated on any device modifications or new protocols.
- Regular refresher courses: Scheduled sessions to reinforce key concepts and update skills.
- Clinical champions/mentors: Designated experts available for on-the-job support and guidance.
- Online resource libraries: Centralized access to manuals, videos, and FAQs for quick reference.
- Feedback mechanisms: Channels for staff to provide input on training effectiveness and needs.
Furthermore, recognizing and rewarding dedication to continuous learning can significantly boost engagement. This could include professional development credits, opportunities for specialization, or internal recognition programs. By investing in their professionals’ growth, healthcare institutions not only enhance competency but also improve job satisfaction and retention.
Leveraging partnerships for enhanced training outcomes
No single entity can shoulder the entire burden of comprehensive MedTech device training. By 2025, successful healthcare organizations will increasingly leverage strategic partnerships with device manufacturers, educational institutions, and specialized training providers to enhance their training outcomes. These collaborations bring specialized expertise, resources, and perspectives that can significantly enrich internal programs.
Device manufacturers, for instance, possess unparalleled knowledge of their products and can offer in-depth training modules, technical support, and updates on device evolution. Educational institutions can provide theoretical foundations and access to advanced simulation facilities, while third-party training providers often bring innovative methodologies and customizable solutions tailored to specific organizational needs.
Collaborating with industry experts
Partnerships with industry experts can bridge knowledge gaps and ensure that training content is always at the cutting edge. These collaborations can take various forms, from co-developing training curricula to hosting joint workshops and webinars. Such initiatives not only improve the quality of training but also foster a broader understanding of the MedTech ecosystem.
- Manufacturer-led training: Direct access to product specialists and up-to-date device information.
- Academic partnerships: Collaboration with universities for curriculum development and research into effective training methods.
- Specialized training vendors: Outsourcing specific training needs to experts with proven methodologies.
- Peer networking: Sharing best practices and resources with other healthcare organizations.
By pooling resources and expertise, healthcare organizations can create more robust, cost-effective, and comprehensive training programs. These partnerships also facilitate knowledge transfer, ensuring that the latest advancements and best practices are quickly integrated into clinical workflows. Ultimately, this collaborative approach is key to achieving and sustaining 100% competency in MedTech device training.
| Key Point | Brief Description |
|---|---|
| Needs Assessment | Identify specific training gaps and target audiences for MedTech devices. |
| Adaptive Curriculum | Develop flexible, technology-integrated training content that evolves with new devices. |
| Competency Validation | Implement robust, multi-faceted assessments to ensure true proficiency and retention. |
| Continuous Learning | Foster a culture of ongoing education, refreshers, and professional development. |
Frequently Asked Questions About MedTech Device Training
Achieving 100% competency is paramount for patient safety, minimizing medical errors, and ensuring optimal clinical outcomes. It also helps healthcare organizations meet stringent regulatory compliance requirements and reduces the risk of device misuse or damage, leading to more efficient operations and better quality of care.
Key steps include conducting a thorough needs assessment to identify gaps, developing an adaptive curriculum incorporating diverse learning methods, implementing robust competency assessment and validation, and fostering a culture of continuous learning. Strategic planning and leveraging external partnerships are also crucial for success.
Technology can significantly enhance training through Learning Management Systems (LMS) for tracking progress, online modules for flexible learning, and immersive tools like virtual reality (VR) and augmented reality (AR) for realistic simulations. Mobile apps can also provide on-demand refreshers and quick guides, making learning accessible and engaging.
Effective assessment methods include written examinations for theoretical knowledge, skills checklists for procedural evaluation, and simulation-based scenarios to test critical thinking and decision-making. Direct observation and peer-to-peer assessments also provide valuable insights into a professional’s proficiency and ability to handle real-world situations.
Partnerships with device manufacturers, educational institutions, and specialized training providers are vital as they offer specialized expertise, resources, and innovative methodologies. These collaborations ensure training content is current, comprehensive, and cost-effective, facilitating knowledge transfer and helping organizations stay ahead of technological advancements and best practices.
Conclusion
Achieving 100% competency in MedTech device training by 2025 is an ambitious yet attainable goal that underpins the future of healthcare. It requires a holistic, strategic approach encompassing meticulous planning, adaptive curriculum development, rigorous assessment, and a steadfast commitment to continuous learning. By embracing technological advancements and fostering collaborative partnerships, healthcare organizations can ensure their professionals are not only proficient but also confident in leveraging medical technology to its fullest potential, ultimately enhancing patient safety and delivering superior care. This journey towards universal competency is an investment in both human capital and the quality of healthcare provided.