FDA Approves 3 New AI Medical Devices for U.S. in Q1 2025

The FDA’s approval of three new AI-powered medical devices for the U.S. market in Q1 2025 heralds a new era in healthcare, promising significant advancements in diagnostics, treatment planning, and patient outcomes.
The landscape of healthcare is on the cusp of a profound transformation. In a landmark announcement, the U.S. Food and Drug Administration (FDA) has granted approval for three new AI-powered medical devices to enter the U.S. market in Q1 2025. This pivotal development, which we are calling Breaking: FDA Approves 3 New AI-Powered Medical Devices for U.S. Market in Q1 2025 – Recent Updates, signifies a monumental step forward in integrating artificial intelligence into clinical practice, promising to redefine diagnostics, personalize treatment strategies, and ultimately improve patient outcomes across the nation. This is not merely an incremental change but a foundational shift that will impact how medical professionals operate and how patients experience care.
The Dawn of a New Era in Medical AI
The FDA’s recent approvals are more than just regulatory milestones; they represent a significant validation of artificial intelligence’s growing role in medicine. For years, AI has been a subject of intense research and development in the healthcare sector, with promises of revolutionizing everything from drug discovery to personalized treatment. Now, these approvals bring those promises closer to reality, demonstrating a maturation of AI technologies capable of meeting stringent safety and efficacy standards.
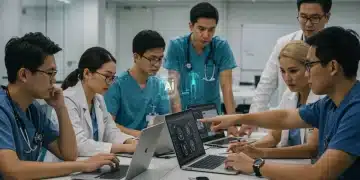
These devices are poised to address some of the most pressing challenges in modern healthcare, including the need for earlier and more accurate diagnoses, more efficient clinical workflows, and tailored therapeutic approaches. The strategic integration of AI is expected to alleviate burdens on healthcare providers, allowing them to focus more on direct patient interaction and complex decision-making, while AI handles intricate data analysis and pattern recognition.
Understanding the FDA’s Rigorous Approval Process
The FDA’s pathway for approving medical devices, especially those incorporating novel technologies like AI, is notoriously rigorous. It involves extensive clinical trials, validation studies, and comprehensive reviews of data to ensure both safety and effectiveness. The fact that these three devices successfully navigated this process speaks volumes about their robustness and the scientific evidence supporting their claims.
- Pre-market Approval (PMA): Often required for high-risk devices, demanding extensive clinical evidence.
- 510(k) Clearance: For moderate-risk devices, demonstrating substantial equivalence to a legally marketed predicate device.
- De Novo Classification: For novel, low-to-moderate risk devices without a predicate, establishing new regulatory controls.
The FDA’s cautious yet progressive approach ensures that while innovation is encouraged, patient safety remains paramount. These approvals reflect a careful balance, acknowledging AI’s potential while mitigating associated risks. This rigorous evaluation instills confidence in both medical professionals and the public regarding the reliability and safety of these advanced tools.
In essence, these approvals signal a clear message: AI is no longer a futuristic concept in medicine; it is a present reality, rigorously vetted and ready to make a tangible difference in patient care. The implications for clinical practice, medical education, and public health are profound and far-reaching.
Deep Dive into the Approved Devices and Their Impact
The three AI-powered medical devices approved by the FDA are set to address critical areas within healthcare, each bringing unique capabilities that promise to enhance existing medical practices. While specific details of the devices are still emerging, their general applications suggest a significant leap forward in precision medicine and diagnostic accuracy.
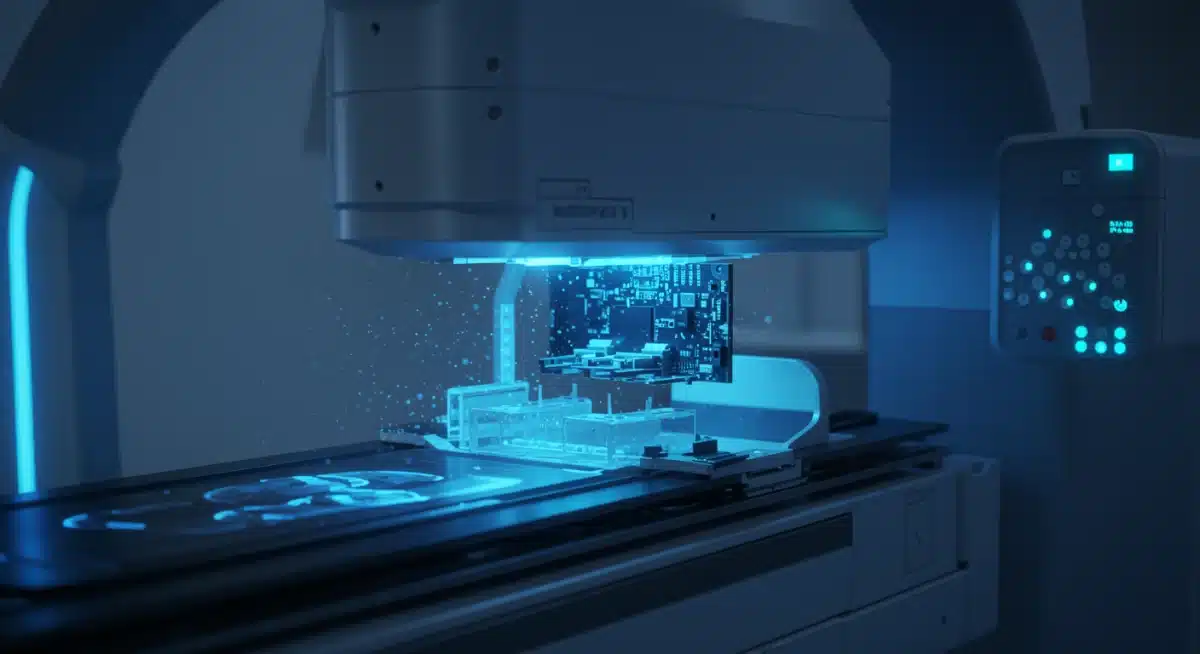
One of the approved devices focuses on advanced diagnostic imaging analysis. This AI system is designed to interpret complex medical images, such as MRIs, CT scans, and X-rays, with remarkable speed and accuracy, often surpassing human capabilities in detecting subtle anomalies. Its ability to identify early indicators of disease could lead to earlier interventions and significantly improved prognoses for patients.

Revolutionizing Disease Detection and Treatment Planning
The second device is an AI-driven platform for personalized treatment planning, particularly in oncology and chronic disease management. This system leverages vast datasets of patient information, including genetic profiles, treatment histories, and real-world outcomes, to recommend optimal therapeutic strategies. It moves beyond a one-size-fits-all approach, enabling clinicians to tailor treatments based on individual patient characteristics, thereby maximizing efficacy and minimizing adverse effects.
- Enhanced Diagnostic Speed: AI can analyze images and data much faster than humans, reducing diagnostic delays.
- Improved Accuracy: Algorithms can detect patterns and anomalies that might be missed by the human eye.
- Personalized Therapies: AI analyzes individual patient data to recommend highly specific and effective treatments.
- Reduced Human Error: Automation of certain tasks can decrease the likelihood of human-induced mistakes.
The third device introduces an AI solution for continuous patient monitoring and predictive analytics in critical care settings. This system constantly analyzes physiological data from various sensors, identifying subtle changes that could indicate impending complications. By providing early warnings, it allows medical teams to intervene proactively, potentially preventing life-threatening events and improving patient safety in intensive care units.
These innovations collectively underscore a paradigm shift where AI acts not just as a supplementary tool, but as an integral partner in clinical decision-making, offering insights and efficiencies that were previously unattainable. The impact on patient care quality and healthcare resource utilization is expected to be substantial.
Anticipated Benefits and Challenges for U.S. Healthcare
The introduction of these three FDA-approved AI medical devices promises a cascade of benefits for the U.S. healthcare system, ranging from improved patient outcomes to enhanced operational efficiencies. However, alongside these promising advancements, there will inevitably be challenges that require careful navigation and strategic planning.
One of the most significant anticipated benefits is the potential for earlier and more precise diagnoses. AI’s ability to process and interpret complex medical data at speeds far exceeding human capacity means that diseases, particularly those with subtle early indicators, can be identified much sooner. This early detection often translates directly into higher success rates for treatment and improved long-term prognoses for patients, reducing the emotional and financial burden of advanced disease stages.
Addressing Data Privacy and Ethical Concerns
Despite the immense promise, the widespread adoption of AI in healthcare also raises important ethical considerations and challenges related to data privacy and security. These AI systems rely on vast amounts of patient data, making robust cybersecurity measures and strict adherence to privacy regulations like HIPAA absolutely critical. Ensuring patient trust requires transparent data handling practices and strong safeguards against breaches.
- Data Privacy: Protecting sensitive patient information from unauthorized access and misuse.
- Algorithmic Bias: Ensuring AI algorithms are fair and do not perpetuate or amplify existing health disparities.
- Physician Training: Equipping healthcare professionals with the skills to effectively use and interpret AI tools.
- Regulatory Frameworks: Adapting existing laws and creating new ones to govern AI in medicine responsibly.
Another challenge lies in the integration of these new technologies into existing healthcare infrastructures. Hospitals and clinics will need to invest in new hardware, software, and significant training for their staff. This transition requires not only financial investment but also a cultural shift within medical institutions to fully embrace AI as a collaborative partner in patient care. Overcoming these hurdles will be crucial for realizing the full potential of these groundbreaking devices.
Ultimately, while the benefits of enhanced diagnostics, personalized treatment, and improved patient monitoring are clear, healthcare stakeholders must collaboratively address the ethical, logistical, and educational challenges to ensure a smooth and equitable integration of AI into the fabric of U.S. healthcare.
Economic Implications and Market Adoption
The FDA’s approval of these three AI-powered medical devices is poised to have substantial economic implications for the U.S. healthcare market. The market for AI in healthcare is already experiencing rapid growth, and these approvals will likely accelerate that trend, attracting further investment and fostering innovation within the medical technology sector.
From a market perspective, these approvals open doors for significant revenue generation for the companies behind these devices, as well as for ancillary businesses involved in their deployment, maintenance, and data integration. This influx of capital and competition is expected to drive down costs in the long run, making advanced AI solutions more accessible to a wider range of healthcare providers. Furthermore, the efficiency gains from AI in diagnostics and treatment planning could lead to substantial cost savings for healthcare systems by reducing misdiagnoses, unnecessary procedures, and prolonged hospital stays.
Investment Trends and Healthcare Spending
The economic landscape will see increased venture capital and private equity flowing into AI healthcare startups, eager to capitalize on the demonstrated regulatory success and market potential. This will fuel further research and development, leading to a new generation of even more sophisticated AI tools. Healthcare providers, too, will face strategic decisions regarding investment in these technologies, weighing the upfront costs against long-term benefits in patient care and operational efficiency.
- Increased Investment: More capital flowing into AI healthcare ventures.
- Market Growth: Expansion of the medical AI market segment.
- Cost Savings: Potential reductions in healthcare expenditures through efficiency.
- Job Creation: New roles in AI development, implementation, and maintenance.
However, the initial adoption phase may present financial barriers for smaller healthcare facilities. The cost of acquiring and integrating these advanced systems, coupled with the need for specialized IT infrastructure and staff training, could be prohibitive for some. Policy makers and industry leaders will need to explore models for equitable access and reimbursement to ensure that the benefits of AI are not limited to well-resourced institutions. The goal must be to democratize access to these cutting-edge tools, ensuring that all patients, regardless of their location or socioeconomic status, can benefit from the advancements.
The economic ripple effect will extend beyond direct sales, influencing insurance policies, healthcare spending patterns, and potentially shifting the focus of medical research. The approvals mark a turning point, solidifying AI as a critical and financially viable component of future healthcare delivery.
The Role of AI in Enhancing Patient Experience and Outcomes
Beyond the technical and economic aspects, the ultimate goal of integrating AI into medicine is to significantly enhance the patient experience and improve health outcomes. The three newly approved AI devices are designed with this core objective in mind, promising to make healthcare more personalized, efficient, and ultimately, more effective for individuals.
One of the most direct impacts on patients will be through more accurate and timely diagnoses. Imagine a scenario where a complex disease is identified months earlier than traditionally possible, leading to treatment before significant progression. This precision can mean the difference between a manageable condition and a life-threatening one. Patients will benefit from reduced diagnostic uncertainty and the anxiety that often accompanies it, leading to a more streamlined and less stressful healthcare journey.
Personalized Care Pathways and Empowerment
The personalized treatment planning capabilities of these AI tools will also empower patients and their physicians. Instead of generic treatment protocols, AI can help craft therapies that are uniquely suited to an individual’s genetic makeup, lifestyle, and specific disease characteristics. This tailored approach not only boosts treatment efficacy but also minimizes side effects, improving quality of life during and after therapy. Patients will feel more involved in their care decisions, understanding that their treatment plan is optimized specifically for them.
- Faster Diagnoses: Reducing waiting times and anxiety for patients.
- Tailored Treatments: Customized therapies leading to better results and fewer side effects.
- Proactive Monitoring: Preventing complications through continuous AI surveillance.
- Improved Communication: AI-generated insights can facilitate clearer discussions between doctors and patients.
Furthermore, AI-powered continuous monitoring devices offer an unprecedented level of vigilance, especially for patients in critical conditions or those managing chronic diseases at home. These systems can detect subtle physiological changes that precede a crisis, alerting healthcare providers and enabling prompt intervention. This proactive approach can prevent readmissions, reduce the severity of adverse events, and provide patients and their families with greater peace of mind regarding their ongoing health management.
In essence, these AI devices are not just technological marvels; they are tools designed to foster a more patient-centric healthcare model. By providing deeper insights, enabling precision care, and ensuring constant vigilance, they are set to significantly elevate the standard of care and empower patients to lead healthier, more fulfilling lives.
Regulatory Outlook and Future of AI in Healthcare
The FDA’s approval of these three AI-powered medical devices is a clear indicator of a progressive regulatory outlook towards artificial intelligence in healthcare. This move sets a precedent and provides valuable insights into how future AI innovations might be evaluated and integrated into clinical practice. It signals a maturation of both the technology and the regulatory bodies tasked with ensuring its safe and effective deployment.
Looking ahead, the FDA is expected to continue refining its regulatory frameworks to keep pace with the rapid advancements in AI. This includes developing clear guidelines for machine learning algorithm updates, ensuring data integrity, and addressing issues of algorithmic bias. The goal is to create a predictable yet flexible pathway for innovators while maintaining the highest standards of patient safety and public health.
Evolving Regulatory Landscape and International Cooperation
The regulatory landscape for AI in healthcare is not static; it is continuously evolving. The FDA is likely to engage in ongoing dialogues with industry experts, academic researchers, and international regulatory counterparts to establish best practices and harmonize standards. This collaborative approach is crucial for fostering global innovation and ensuring that AI medical devices meet universal benchmarks for safety and efficacy.
- Adaptive Regulations: Frameworks will evolve to accommodate AI’s dynamic nature.
- Global Standards: Increased cooperation to harmonize AI medical device regulations worldwide.
- Post-Market Surveillance: Enhanced monitoring of AI devices after approval for continuous safety assessment.
- Ethical AI Development: Focus on guidelines that ensure fairness, transparency, and accountability in AI algorithms.
The future of AI in healthcare will also heavily depend on continued research and development, especially in areas like explainable AI (XAI), which aims to make AI decisions more transparent and understandable to human users. This will be vital for building trust among clinicians and patients alike. Furthermore, the integration of AI with other emerging technologies, such as genomics and personalized medicine, promises an even more transformative impact, creating a holistic approach to health and wellness.
In conclusion, these FDA approvals are not just about three devices; they represent a significant step in the ongoing journey of integrating AI into mainstream medicine. The regulatory bodies, innovators, and healthcare providers must work in concert to navigate this future, ensuring that AI contributes positively and ethically to the health and well-being of populations worldwide.
Preparing for the AI Revolution in Clinical Practice
The imminent arrival of these FDA-approved AI medical devices necessitates significant preparation within clinical practice across the United States. Healthcare institutions, from large hospital systems to individual clinics, must begin strategizing how to effectively integrate these advanced tools into their daily operations and clinical workflows. This preparation goes beyond just acquiring the technology; it involves a comprehensive approach to training, infrastructure, and cultural adaptation.
One of the most critical aspects of preparation is the education and training of healthcare professionals. Physicians, nurses, radiologists, and other clinical staff will need to understand how these AI devices function, how to interpret their outputs, and how to seamlessly incorporate them into diagnostic and treatment pathways. This will likely involve specialized workshops, continuing medical education (CME) courses, and hands-on training sessions to build confidence and competence in using AI.
Infrastructure Upgrades and Workflow Optimization
Beyond human capital, robust technological infrastructure will be essential. This includes upgrading IT systems to handle the massive data processing requirements of AI, ensuring secure and interoperable data exchange, and establishing protocols for data management and storage. The goal is to create an ecosystem where AI tools can operate efficiently and securely, without disrupting existing critical healthcare systems.
- Staff Training: Comprehensive programs for all relevant healthcare professionals.
- IT Infrastructure: Upgrades to support AI data processing and integration.
- Workflow Redesign: Adapting clinical processes to leverage AI efficiencies.
- Ethical Guidelines: Development of internal policies for responsible AI use.
Healthcare organizations will also need to re-evaluate and optimize their clinical workflows to maximize the benefits of AI. This might involve redesigning diagnostic pathways, streamlining patient intake processes, or automating certain administrative tasks to free up clinician time. The aim is to leverage AI to enhance efficiency, reduce burnout, and allow healthcare providers to dedicate more attention to complex patient needs and compassionate care.
The successful integration of these AI devices will require a proactive and adaptive mindset from all stakeholders. By investing in training, infrastructure, and thoughtful workflow redesign, U.S. healthcare can fully embrace the potential of AI to revolutionize patient care, leading to a more efficient, accurate, and personalized medical future.
| Key Point | Brief Description |
|---|---|
| FDA Approvals | Three new AI-powered medical devices approved for U.S. market in Q1 2025. |
| Device Focus | Advanced diagnostic imaging, personalized treatment, and critical care monitoring. |
| Anticipated Impact | Earlier diagnoses, tailored treatments, improved patient outcomes, and operational efficiency. |
| Challenges Ahead | Data privacy, algorithmic bias, physician training, and infrastructure integration. |
Frequently Asked Questions About AI Medical Device Approvals
AI-powered medical devices utilize artificial intelligence, including machine learning and deep learning algorithms, to assist in various medical tasks. These can range from analyzing medical images for diagnostic purposes to predicting disease progression, personalizing treatment plans, and monitoring patient health with enhanced precision and efficiency.
The FDA employs a rigorous approval process that includes extensive pre-clinical and clinical testing, data validation, and comprehensive reviews of a device’s performance. For AI devices, this also involves assessing the algorithms for accuracy, reliability, and potential biases, ensuring they meet stringent safety and efficacy standards before market entry.
The newly approved devices are expected to impact diverse medical areas. One focuses on advanced diagnostic imaging for various diseases, another on personalized treatment planning for conditions like cancer, and a third on continuous patient monitoring in critical care. This broad scope targets enhancing care across multiple specialties.
No, AI medical devices are designed to augment, not replace, human doctors. They serve as powerful tools to assist clinicians in making more informed decisions, enhancing diagnostic accuracy, and streamlining workflows. The human element of empathy, complex reasoning, and direct patient interaction remains indispensable in healthcare.
Key ethical concerns include ensuring patient data privacy and security, preventing algorithmic bias that could exacerbate health disparities, establishing clear accountability for AI-driven decisions, and maintaining transparency in how AI systems function. Addressing these issues is crucial for building trust and ensuring equitable access to AI benefits.
Conclusion
The FDA’s approval of three new AI-powered medical devices for the U.S. market in Q1 2025 marks a pivotal moment in healthcare innovation. These advancements promise to usher in an era of more precise diagnostics, highly personalized treatment strategies, and proactive patient care, fundamentally transforming the medical landscape. While the journey ahead involves navigating challenges related to data privacy, ethical considerations, and systemic integration, the potential benefits for patients and healthcare providers are immense. This development underscores a future where artificial intelligence is not merely a technological aid but a cornerstone of advanced, compassionate, and efficient medical practice, ultimately leading to improved health outcomes for millions.